
Concussion Management: Does marijuana play a role?
Published on: October 19, 2018
 Recently more and more questions have arisen regarding the use of marijuana as a rehabilitation intervention following a concussion. For example, some patients may ask if marijuana can help rid symptoms of headaches, inability to sleep, or anxiety. Other patients might say they are regular legal users of marijuana, and wonder if they should increase their intake medicinally, or if they should refrain from their normal daily usage while recovering from a concussion.
Recently more and more questions have arisen regarding the use of marijuana as a rehabilitation intervention following a concussion. For example, some patients may ask if marijuana can help rid symptoms of headaches, inability to sleep, or anxiety. Other patients might say they are regular legal users of marijuana, and wonder if they should increase their intake medicinally, or if they should refrain from their normal daily usage while recovering from a concussion.
These are all extremely relevant questions that many members of the healthcare community are learning as more research becomes available. To date some 20 states plus Washington D.C. have successfully enacted cannabis-related medical marijuana legislation whereby the substance must be prescribed by a licensed physician. Additionally, 9 states, Washington D.C. and now Canada have passed laws legalizing recreational use of marijuana, despite the fact that it still remains illegal on a federal level.
The down and dirty is that there are essentially two types of natural compounds derived from the cannabis plant: cannabidiol (CBD) and tetrahydrocannabinol (THC). CBD comes in the form of gels, oils, gummies and supplemental extracts, while THC is most commonly inhaled by smoking, it is available in oils, tinctures, and even edible forms such as capsules. Both CBD and THC obviously impact brain function, but it is THC that claims a psychoactive component whereby its use leads to a euphoric or “high” state of mind.
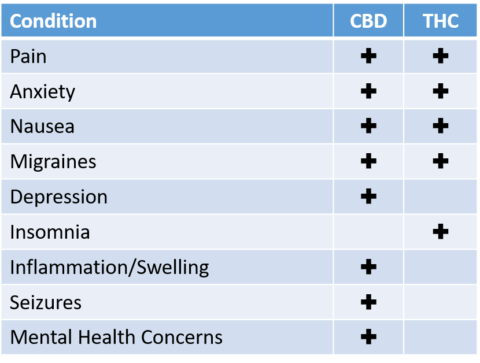
A compilation of sources note that each is commonly used for the following concussion-related conditions:
The reported side effects of CBD are largely attributed to drug interactions when it is combined with other medications. Whereas with THC, memory loss and slower reaction times may be a result of usage, with the possibility of more long-term adverse psychoactive effects with extended use of high dosages.
Since marijuana is relatively new in the game when we discuss its role with concussion management, there seems to be two very strong camps of opinion – “pro” marijuana physicians and other similar healthcare providers clearly support marijuana as an effective intervention. Others who oppose the use of marijuana on all of its merits have not at all been convinced or are willing to consider any positive role that it may play in the facilitation of healing and recovery post-concussion.
One of the pro camp beliefs supporting the use of marijuana after a concussion is the fact that there is evidence demonstrating a protection of neural damage, thus enabling a more rapid healing process of the brain. However, much more research needs to be done before we reach a tipping point beyond mere extrapolation and inference.
There is one interesting study that was published by Nguyen et al in The American Surgeon in 2014 where the authors concluded that patients who sustained a concussion as the result of an automobile accident and had traces of THC in their bloodstream were less likely to experience a fatal outcome from the trauma.
As we become more knowledgeable and evaluate future independent randomized controlled studies, we will likely learn not just generically whether there are benefits or not to the use of marijuana in concussion recovery, but more so hopefully more specificity regarding specific strands of marijuana, dosage, and symptomatic decision-making. As with all contemporary interventions, the question still remains unanswered regarding the role that marijuana plays, if any, with concussions. Be prepared for an increase in research regarding the relationship between marijuana usage and concussion rehabilitation. Also be prepared for mixed findings of results, and some great debates in the near future!