CASE STUDY: Home-based Vestibular Rehabilitation (VRT) Program: Measuring Outcomes with vHIT and Dynamic Visual Acuity Tests
Published on: March 11, 2015
Vestibular Rehabilitation Therapy (VRT) is well established as the gold standard for the non-medical management of chronic non-compensated unilateral vestibulopathy secondary to acute onset otologic conditions or vestibular migraine. The question often arises whether a home-based program can provide successful outcomes for those patients unable or unwilling to participate in a clinician directed program in an outpatient or hospital rehabilitation services department. A typical clinic-based program requires 2-3 visits per week for 3-4 weeks. Even with the best clinician directed VRT, therapy should be supplemented daily with home exercises to ensure maximum benefit. For selective patients and health systems, a home-based program may offer a less obtrusive and more cost effective method for recovering function and returning to a normal lifestyle or employment. It is critical however to validate the patient’s recovery through objective measures, particularly for those whose subjective reporting may be biased by their enthusiasm or financial need to return to work or play.
CASE STUDY: A 66-year-old male Cruise ship educator/entertainer experienced acute onset debilitating vertigo without any other auditory or focal neurological symptoms while the ship was underway at sea. Once back home, a family physician, as well as an otologist diagnosed the patient with a likely vestibular neuritis. MRI with contrast was negative. After not benefiting from a spontaneous compensation he was referred to AIB for evaluation and management 4 weeks post event. He was anxious to return to his ship, as this was an unpaid sick leave, but could not in his present state. Likewise, his insurance would not cover outpatient physical therapy. The use of a home-based program using Diagnosis Based Strategies was the best management strategy for this patient. His predominate complaints were: blurred vision with head movement in horizontal plane, imbalance on uneven or dynamic surfaces and motion intolerance (which he had never experienced from his daily Cruise ship livelihood).
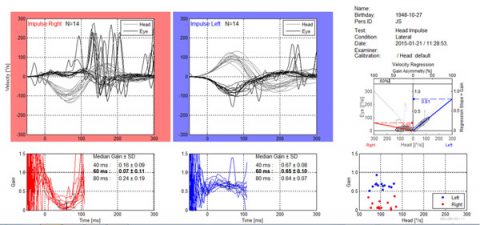
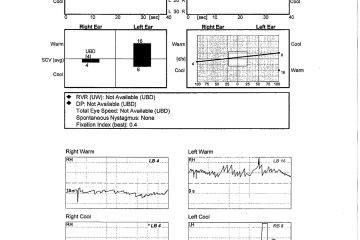
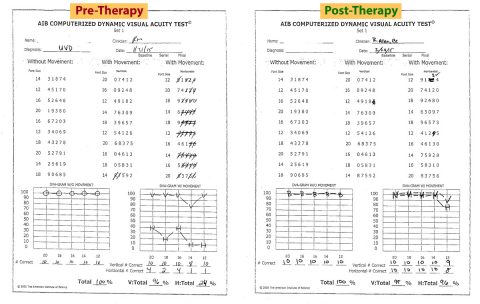
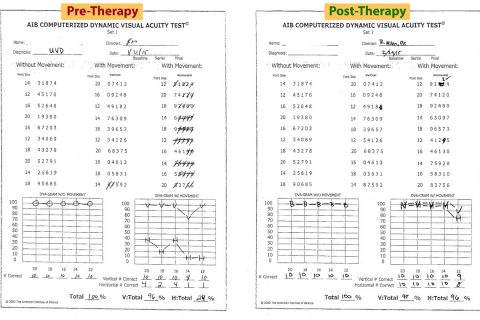
Initial Findings: Abnormal results: Gans SOP (Fall on CTSIB- condition six), VNG-83% right unilateral weakness, rotary chair- low gain bilaterally, vHIT– abnormal with corrective saccades to the right and AIB CDVAT reduced from 100% to 24% with horizontal head movement at 2 cps. Several of the studies are presented for your review.
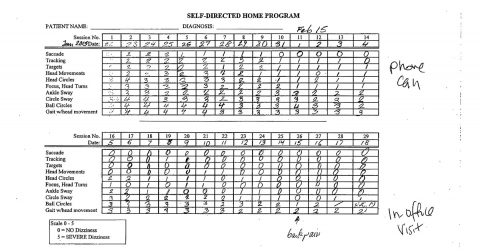
VRT Home Based Program: The patient was provided with a VRT program, which had been customized for his specific needs to address the non-compensated conditions, which manifested as oscillopsia, vestibular recruitment and surface/visual preference. Therefore he required gaze stabilization, habituation and substitution protocols. He was provided with a daily diary-self monitoring system to record his performance and subjective experience.
Post VRT testing and Recommendations: 4 weeks post treatment, as can be seen in the review of post VRT testing, there is a statistically significant improvement on the AIB CDVAT with a near complete resolution of the oscillopsia with Dynamic Visual Acuity score back to 96%. There was also a significant but not total elimination of corrective saccades on vHIT. Since the corrective saccade is the physiological manifestation of the oscillopsia, one would expect to see this relationship. Postural stability on Gans SOP also was improved. Note the subjective report on the patient’s diary with a significant reduction in the intensity of symptoms with the protocols. Based on these objective findings and the patient’s subjective report of full recovery by virtue of elimination of symptoms, he was discharged and allowed to return to work aboard the Cruise ship. He was encouraged to continue his home-based protocols for at least the next 2-3 weeks. In addition possible de-compensation was discussed secondary to other factors such as illness or sedentary lifestyle.
Take Home Message:
1. Home based VRT produces excellent outcomes when utilized with the proper individual who is not at risk for injury or where it is not medically contraindicated without a trained therapist.
2. The use of a diary or self monitoring system is helpful to both patient and clinician in following patient’s progress and ensuring a step-wise progression of increasingly difficult protocols.
3. vHIT, CTSIB and Dynamic Visual Acuity Tests are reliable and have high sensitivity for validation of central compensation in individuals who may be too enthusiastic to return to their duties without the use of subjective outcome measures.
REFERENCES
Gans R., (2015) Vestibular Rehabilitative Therapy In Katz J., Chasin. M., English, K., Hood L., Tillery K.L. (Eds.) Handbook of Clinical Audiology 7th Edition. Philadelphia: Wolters Kluwer Heath
Gans, R., (2013) Vestibular Rehabilitation Therapy. (2013) In: Dispenza F, De Stefano A, (Eds.) Textbook of Vertigo Diagnosis and Management. London: Jaypee Brothers Medical Publishers
Gans R, (2010) Vestibular Rehabilitation: protocols and Programs. Tampa Bay, AIB Education Press
Roberts RA, Gans RE (2007) Comparison of horizontal and vertical dynamic visual acuity in patients with vestibular dysfunction and nonvestibular dizziness. J Am Acad Audiol. 18, 236-244
Roberts RA, Gans RE, Johnson EL (2006) Computerized dynamic visual acuity with volitional head movements in patients with vestibular dysfunction. Ann Otol Rhinol Laryngol. 115(9), 658-666